The importance of iron for whole blood donors: a Canadian perspective
Authors: Aditi Khandelwal, MDCM, MSc, FRCPC, DRCPSC; Chantale Pambrun, MD, FRCPC and Mindy Goldman, MD, FRCPC
Primary target audiences: medical laboratory technologists, transfusion nurses, transfusion safety officers, physicians, Patient Blood Management programs
Published: March 28, 2017, updated February 8, 2023
Key points
-
Iron deficiency is common in whole blood donors, particularly female donors, frequent donors, and donors failing their hemoglobin (Hb) screening test.
-
Since 2017, Canadian Blood Services has increased the donation interval for female whole blood donors to 84 days (from 56 days) and increased the hemoglobin threshold for male whole blood donors from 125g/L to 130g/L to reduce the risk of iron deficiency in these donors.
-
In 2023, Canadian Blood Services started ferritin testing in select frequent whole blood donors at the highest risk of iron deficiency.
-
Whole blood donors should speak to their physician about iron supplementation to replenish lost iron stores from blood donation. A diet rich in iron is recommended for all blood donors but this may not be sufficient to restore normal ferritin levels.
-
Physicians should order serum ferritin levels on patients who are frequent whole blood donors (more than three whole blood donations per year for males and more than one whole blood donation per year for females).
-
Physicians should consider iron supplementation in all patients that are blood donors. A daily supplement (37.5 mg of elemental iron) for 8 weeks should be sufficient to replenish iron losses from a whole blood donation.
Introduction
By generously providing blood that can be manufactured into red blood cells, platelets and plasma components, whole blood donors are essential to the blood system and the patients it serves. Canadian Blood Services is committed to maintaining a safe and secure blood supply while also protecting the health of our blood donors. This article examines the effect of red blood cell loss on donor iron levels and the steps taken by Canadian Blood Services to protect the health of its donors.
Red blood cells are the most abundant cell type in blood. They are packed with hemoglobin, which is responsible for transporting oxygen throughout the body and removing carbon dioxide. Iron is a vital building block of hemoglobin; each hemoglobin molecule is composed of four iron atoms. Iron is an essential element obtained through diet and used for biochemical functions throughout the body. This can be illustrated with a passenger car and ferry analogy: the iron provides the seat for oxygen in the hemoglobin vehicle, which is transported in the red blood cell ferry. The ferry delivers its cargo to organs and tissues, after travelling through arteries, veins and capillaries.
Iron stores in the body
Iron is stored in liver cells as well as within a protein shell called ferritin. Measuring serum ferritin can help estimate iron stores in the body. Whole blood donors are required to pass a fingerpick hemoglobin screening test using a portable hemoglobinometer; however, ferritin testing is not available at blood donor clinics.
Cooper et al. (2012) report that the prevalence of sufficient serum ferritin for Canadians in the 20- to 49-year-old age group is 98.7% for males sex-at-birth (95% confidence interval [CI] 97.5–99.9) and 90.9% for females sex-at-birth (95% CI 87.2–94.6).1 Females have lower ferritin levels, with the highest prevalence of insufficient serum ferritin amongst those in the 12 to 19 years age range (13%).1 With a single whole blood donation of 500 mL, there is an expected loss of 225–250 mg of iron. This loss may lead to health problems if not replenished through diet and/or iron supplementation. It is estimated that up to 35% of whole blood donors become iron-deficient (defined as ferritin below 25 µg/L (see Table 1) from regular whole blood donation.2 Iron supplementation (37.5 mg of elemental iron) consumed daily for eight weeks is expected to replenish the iron loss from one whole blood donation.2
Symptoms of iron deficiency with or without anemia
Iron deficiency can occur with or without anemia (i.e., low hemoglobin). The current donor hemoglobin screening process at Canadian Blood Services will detect and defer donors who have anemia but not those who have iron deficiency without anemia (IDWA). The broad range of symptoms related to iron deficiency is attributed to the many physiological uses of iron.
If IDWA is not treated, it may progress to iron deficiency anemia. It is important for blood donors and their physicians to be aware of the link between whole blood donation and iron deficiency to avoid unnecessary diagnostic tests for otherwise-healthy individuals developing iron deficiency after blood donation.3-5
Iron deficiency without anemia
Symptoms of IDWA have mainly been studied in premenopausal women. One-fourth of menstruating women have iron deficiency; fatigue is the most commonly reported symptom.6-11 In IDWA, fatigue improves with iron repletion.11 Iron depletion is associated with fatigue, decreased exercise capacity, neurocognitive changes, pica and restless leg syndrome2,12 and IDWA impairs quality of life.6,13,14
Iron deficiency anemia
The physiological manifestations of iron deficiency anemia include reduced immune function, impaired cognitive performance, behaviour changes, decreased thermoregulatory performance and energy metabolism, and diminished exercise or work capacity.15,16
Table 1: Iron status by serum ferritin levels*
| Iron status | Serum ferritin levels |
|---|---|
| Absent iron stores | < 12 µg/L |
| Low iron stores | 12–24 µg/L |
| Adequate iron stores | > 25 µg/L |
| *The clinical definition of iron deficiency can vary depending on the guidelines being followed and the clinical context. The ferritin value corresponding to iron deficiency as a medical diagnosis may vary from <12 ug/L to <40 ug/L in those without underlying chronic illness or inflammation.17 | |
Iron status of Canadian Blood Services’ whole blood donors
Canada’s fresh blood components are provided by approximately 415,000 volunteer donors. Each year, Canadian Blood Services collects approximately 800,000 units of whole blood. A dedicated group of repeat donors provides close to 92% of donations, while 8% of donations come from first time donors.18 The average whole blood donation frequency in 2021 was slightly over two donations per donor yearly.
Donor hemoglobin screening is performed on a fingerstick capillary sample prior to each whole blood donation, with a minimum qualifying level of 125 g/L required for female donors and 130 g/L for male donors. In 2018, 8% of female donors and 2% of male donors were temporarily deferred from donation for a low hemoglobin level. A low hemoglobin level can be a late consequence of iron depletion but may also, less commonly, be due to other causes (e.g., vitamin B12 deficiency, bone marrow pathology).
As of January 2023, Canadian Blood Services has started selectively testing donor iron stores.19 There is increasing evidence that whole blood donation may cause iron deficiency, particularly in female and frequent male donors.3,4,20-22 At Canadian Blood Services, the hemoglobin-related donor deferral rate increases with frequency of whole blood donation. The correlation between blood donor status and iron deficiency may be under-recognized both by donors and their physicians.3-5 Iron status is recognized as a donor safety issue based on the associated symptoms of iron depletion discussed above.
Canadian Blood Services performed studies to assess the prevalence of iron deficiency in its whole blood donors by measuring ferritin levels in approximately 13,000 donors (i.e., 2.6% of our donor base) (see Table 2).21,23,24 Donors with low ferritin received an information sheet and a letter advising them to see their physician or pharmacist about starting iron supplementation. In addition, we evaluated donors’ knowledge of the impact of blood donation on their iron levels and assessed the discussions that they may have had with their family physician about iron health and blood donation.
The main findings of the studies were:
- Donor knowledge about iron is poor and few donors discuss blood donation with their physician.
- Repeat donors are often iron deficient despite passing a hemoglobin screen.
- Most donors failing their hemoglobin screen are iron deficient.
- Donors with low ferritin are not always advised to take iron supplements by their physician.
- Many donors will start iron supplementation if advised to do so by their physician.
Table 2: Ferritin levels in study donors by sex*. Table adapted from Goldman et al. (2017).23
| Ferritin level (µg/L) | ||||||||||
| Sex | Age (years) |
Donation status |
Donation frequency in past 12 months† |
Donors | Hb (g/L) | Ferritin (µg/L) | <12 | 12-24 | 25-336 | >336 |
|---|---|---|---|---|---|---|---|---|---|---|
|
Female |
17-24 |
First-time/ |
|
514 (9.1) |
141 (140-142) |
33 (31-35) |
64 (12.5) |
169 (32.9) |
281 (54.7) |
|
|
Repeat |
1-2 donations |
358 (6.3) |
137 (136-139) |
18 (17-20) |
163 (45.5) |
101 (28.2) |
94 (26.3) |
|
||
|
3 donations |
68 (1.2) |
136 (134-138) |
12 (9-15) |
49 (72.1) |
15 (22.1) |
4 (5.9) |
|
|||
|
≥4 donations |
38 (0.7) |
139 (135-142) |
18 (11-24) |
20 (52.6) |
9 (23.7) |
9 (23.7) |
|
|||
|
25-45 |
First-time/ |
|
824 (14.6) |
139 (138-140) |
44 (40-47) |
65 (7.9) |
205 (24.9) |
553 (67.1) |
1 (0.1) |
|
|
Repeat |
1-2 donations |
803 (14.2) |
138 (138-139) |
24 (22-25) |
232 (28.9) |
291 (36.2) |
280 (34.9) |
|
||
|
3 donations |
224 (4.0) |
138 (136-139) |
17 (15-19) |
100 (44.6) |
78 (34.8) |
46 (20.5) |
|
|||
|
≥4 donations |
163 (2.9) |
136 (134-139) |
17 (15-20) |
78 (47.9) |
55 (33.7) |
30 (18.4) |
|
|||
|
≥46 |
First-time/ |
|
561 (9.9) |
141 (140-142) |
67 (62-72) |
31 (5.5) |
78 (13.9) |
450 (80.2) |
2 (0.4) |
|
|
Repeat |
1-2 donations |
1052 (18.7) |
140 (140-141) |
33 (31-35) |
175 (16.6) |
309 (29.4) |
567 (53.9) |
1 (0.1) |
||
|
3 donations |
446 (7.9) |
140 (139-141) |
25 (22-27) |
130 (29.1) |
174 (39.0) |
142 (31.8) |
|
|||
|
≥4 donations |
589 (10.4) |
139 (138-140) |
20 (18-21) |
219 (37.2) |
237 (40.2) |
133 (22.6) |
|
|||
|
|
Total |
|
5640 (100.0) |
139 (139-140) |
32 (31-33) |
1326 (23.5) |
1721 (30.5) |
2589 (45.9) |
4 (0.1) |
|
|
Male |
≥17 |
First-time/ |
|
1502 (26.6) |
156 (155-156) |
126 (121-132) |
8 (0.5) |
35 (2.3) |
1391 (92.6) |
68 (4.5) |
|
Repeat |
1-3 donations |
3287 (47.3) |
153 (153-154) |
58 (55-60) |
225 (6.8) |
665 (20.2) |
2367 (72.0) |
30 (0.9) |
||
|
4-5 donations |
1978 (28.4) |
150 (149-151) |
28 (26-29) |
527 (26.6) |
708 (35.8) |
739 (37.4) |
4 (0.2) |
|||
|
≥6 donations |
188 (2.7) |
149 (147-151) |
21 (18-24) |
64 (34.0) |
81 (43.1) |
43 (22.9) |
|
|||
|
|
Total |
|
6955 (100.00) |
153 (153-153) |
63 (61-65) |
824 (11.8) |
1489 (21.4) |
4540 (65.3) |
102 (1.5) |
|
|
* Data are reported as number (%) or mean (95% CI). |
||||||||||
These results in Canadian donors are similar to those seen in studies performed in the U.S., Australia, Switzerland, the Netherlands, and Denmark.20-27 As in other countries, donor sex-at-birth and frequency of donation were the main determinants of iron deficiency in whole blood donors.20,25-27
Notifying donors about their iron deficiency was effective and resulted in a lower donation frequency in the two-year follow-up period, compared to donors with normal ferritin levels (who were not notified) similar to the findings of the STRIDE study.28 Qualitative interviews with donors revealed that general comprehension about the relationship between hemoglobin and iron was poor, donors were not well informed to deal with the side effects of iron therapy, and their discussions with physicians were often limited and occurred at their annual check-up.
These internal studies combined with results from international studies were the basis for implementing iron deficiency mitigation steps, including selective ferritin (iron stores) testing,19 at Canadian Blood Services.
Iron deficiency mitigation steps at Canadian Blood Services
Our studies demonstrated that the majority of whole blood donors who fail their hemoglobin screen have low (12–24 µg/L ferritin) or absent (< 12 µg/L ferritin) iron stores. Investigations may include repeat hemoglobin measurement on a venous sample, which is more accurate than the fingerstick hemoglobin performed on a portable hemoglobinometer in donor clinics. Follow-up testing may include an individualized assessment of factors contributing to lower hemoglobin, including a serum ferritin level. Other investigations may be appropriate and individualized by the health-care practitioner and should consider a variety of factors including the patient’s age, menstrual status, pregnancy history, family history of gastrointestinal cancer, and the presence of any symptoms or signs of other possible underlying conditions contributing to blood loss or impaired nutrient absorption. Guidelines developed by the British Society of Gastroenterology recommend obtaining a history of blood donation as part of the investigation of iron deficiency.29
A trial of iron supplementation, temporary cessation of blood donation, and another evaluation of hemoglobin and ferritin after six months may be appropriate in younger blood donors, while a gastrointestinal investigation may be indicated in a first-time, older donors. Those with a personal or family history of hemochromatosis should not be on iron supplementation.
On the information sheet (Figure 1), donors who fail their hemoglobin screen are advised not to return to donate until they have seen their physician and determined the cause of the anemia. If donors are placed on iron supplementation for iron deficiency anemia, they are advised not to return to donate until they have completed six months of iron supplementation and the iron deficiency anemia has resolved.
Since iron deficiency is so common amongst whole blood donors, we recommend that donors and physicians discuss blood donations during regular check-up visits. Individuals with possible symptoms of iron deficiency, such as unexplained fatigue, should have serum ferritin levels measured. Additionally, younger donors (age <20 years), or individuals who are donating two or more times per year, should have serum ferritin levels measured.30-33
To replace one whole blood donation,34 daily elemental iron supplementation of 37.5 mg for at least eight weeks is required. For individuals donating on a regular basis, particularly in individuals who are menstruating or have had recent pregnancy/pregnancies, it is very difficult to replace the amount of iron lost in donation by diet alone or by multivitamins that do not contain sufficient amounts of iron.6 Table 3 shows some iron preparations available in Canada, and the number of tablets necessary to replace the iron lost in each whole blood donation. In most studies of iron supplementation in blood donors, donors have been advised to take one tablet daily at bedtime, preferably at least two hours after dinner on an empty stomach, for up to a three-month period per donation to replace iron loss. Individuals starting with low iron stores (Table 1) will require a longer period of iron supplementation to replenish their iron reserves.
As shown in our study and by Statistics Canada, many donors registered as female sex-at-birth already have depleted iron reserves before starting to donate blood. Donors who take at least 37.5 mg of elemental iron supplementation return to their pre-donation hemoglobin levels faster (4–5 weeks) versus those who did not take an iron supplement (11–23 weeks).2 Oral iron supplementation for eight weeks has been shown to improve total body iron after a whole blood donation.35 Individuals taking iron supplements who have been diagnosed with iron deficiency without anemia are advised to resume donation after their iron stores have been repleted (ferritin ≥ 25mcg/L)
Table 3: Iron supplements available in Canada.
| Iron preparation | Tablet (mg) | Elemental iron (%) | Elemental iron per tablet (mg) |
No. tablets, 2000 mg total dose | No. tablets, 4000 mg total dose |
|---|---|---|---|---|---|
| Ferrous sulfate | 300 | 20 | 60 | 33 | 66 |
| Ferrous gluconate | 300 | 11.6 | 35 | 57 | 114 |
| Ferrous fumarate | 300 | 33 | 99 | 20 | 40 |
| Polysaccharide - iron complex | 150 | 100 | 150 | 14 | 28 |
Alternative sources of iron
Several alternative sources of iron are available (in addition to food sources, multivitamins and supplementation). A few of these alternatives include mineral water and cooking solutions (e.g., cast iron cookware, Lucky Iron Fish, Lucky Iron Leaf). Individuals are reminded to consult with a physician or pharmacist to determine if an adequate amount of iron is available through these alternatives for their particular situation. As noted above, frequent whole blood donors, young donors (age 25 years and under), menstruating individuals and women require more iron than the recommended daily intake to maintain adequate iron stores (see Table 1). In healthy individuals, there is no anticipated harm in using these alternatives. However, the efficacy of these alternatives for the prevention and treatment of iron deficiency has not been shown in developed countries.
Starting Jan 2023, some donors will have their ferritin level tested. Initially, this testing strategy is being applied to whole blood donors registered as female at every tenth donation.19 If the donor has iron deficiency (ferritin <25ug/L), they will be advised to pause from donation for six months, replenish their iron stores and be assessed by their healthcare practitioners. The strategy to inform donors of their iron status with the goal to help empower them to maintain their iron health has been demonstrated to be effective in multiple studies.24,28 This is the latest incremental step in addressing iron health in donors and will be evaluated further for expansion.
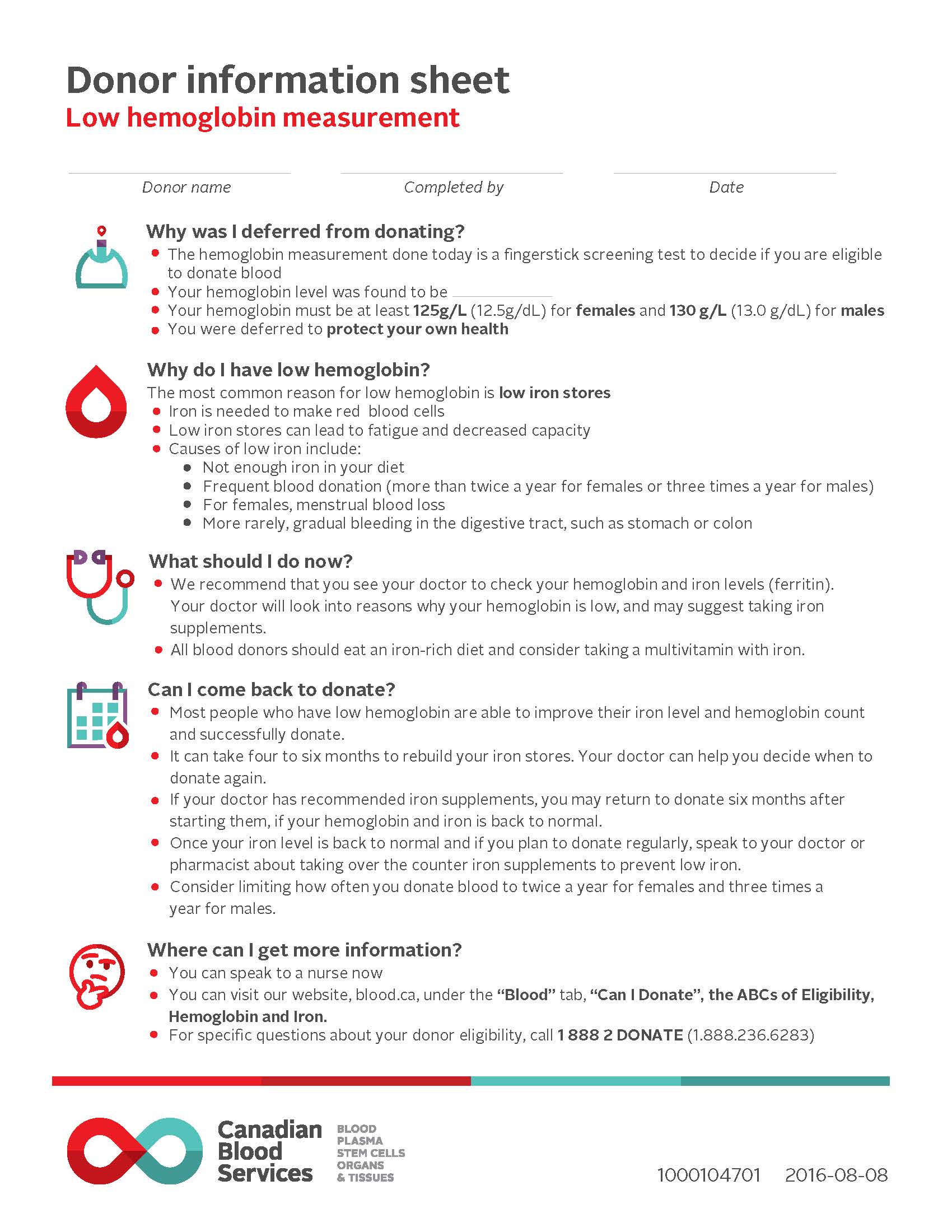
Figure 1: Donor information sheet. This is an example of the information sheet provided to a donor when they do not meet the lower hemoglobin threshold to proceed with a blood donation. This additional tool for sharing information about hemoglobin and iron with donors suggests strategies to help address the decreased hemoglobin level. Donors can also share this sheet with their healthcare practitioner.
Conclusion
Our blood system is supported entirely by voluntary donations made by approximately two per cent of Canadian adults who selflessly enable lifesaving treatments for all by donating blood. Iron deficiency is a common problem in Canada, particularly in women of child-bearing age. Whole blood donation has a significant impact on iron stores in frequent donors, particularly females. Several measures are necessary to prevent, detect, and treat iron deficiency in donors. Canadian Blood Services has implemented several strategies to mitigate the risk of iron loss through whole blood donation, including reduction in the frequency of whole blood donations by donors most susceptible to iron deficiency, better educating both donors and their physicians about iron depletion associated with whole blood donation and selectively testing ferritin in some donors. Frequent donors are encouraged to discuss blood donation and possible need for ferritin monitoring and iron supplementation with their physicians. Conversely, when assessing iron deficiency or nonspecific symptoms associated with iron deficiency such as fatigue, physicians should ask their patients about blood donation. Regular blood donors may require temporary iron supplementation to replenish the iron lost from blood donation.
Suggested citation
Khandelwal A, Pambrun C, Goldman M. The importance of iron for whole blood donors: A Canadian perspective [Internet]. Ottawa: Canadian Blood Services; 2023 [cited YYYY MM DD]. Available from: The importance of iron for whole blood donors: a Canadian perspective | Professional Education
References
- Cooper, M., Greene-Finestone, L., Lowell, H., et al. Iron sufficiency of Canadians. Health Rep 23, 41-48 (2012).
- Kiss, J.E., Brambilla, D., Glynn, S.A., et al. Oral iron supplementation after blood donation: a randomized clinical trial. Jama 313, 575-583 (2015).
- Brittenham, G.M. Iron deficiency in whole blood donors. Transfusion 51, 458-461 (2011).
- Popovsky, M.A. Anemia, iron depletion, and the blood donor: it's time to work on the donor's behalf. Transfusion 52, 688-692 (2012).
- AABB. Updated strategies to limit or prevent iron deficiency in blood donors. in Association Bulletin #17-02, (2017).
- Krayenbuehl, P.A., Battegay, E., Breymann, C., et al. Intravenous iron for the treatment of fatigue in nonanemic, premenopausal women with low serum ferritin concentration. Blood 118, 3222-3227 (2011).
- Vaucher, P., Druais, P.L., Waldvogel, S., et al. Effect of iron supplementation on fatigue in nonanemic menstruating women with low ferritin: a randomized controlled trial. CMAJ 184, 1247-1254 (2012).
- Verdon, F., Burnand, B., Stubi, C.L., et al. Iron supplementation for unexplained fatigue in non-anaemic women: double blind randomised placebo controlled trial. BMJ 326, 1124 (2003).
- Waldvogel, S., Pedrazzini, B., Vaucher, P., et al. Clinical evaluation of iron treatment efficiency among non-anemic but iron-deficient female blood donors: a randomized controlled trial. BMC Med 10, 8 (2012).
- Al-Naseem, A., Sallam, A., Choudhury, S., et al. Iron deficiency without anaemia: a diagnosis that matters. Clin Med (Lond) 21, 107-113 (2021).
- Kassebaum, N.J., Jasrasaria, R., Naghavi, M., et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood 123, 615-624 (2014).
- Pratt, J.J. & Khan, K.S. Non-anaemic iron deficiency - a disease looking for recognition of diagnosis: a systematic review. Eur J Haematol 96, 618-628 (2016).
- Bruner, A.B., Joffe, A., Duggan, A.K., et al. Randomised study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet 348, 992-996 (1996).
- Murray-Kolb, L.E. & Beard, J.L. Iron treatment normalizes cognitive functioning in young women. Am J Clin Nutr 85, 778-787 (2007).
- Beard, J.L., Dawson, H. & Pinero, D.J. Iron metabolism: a comprehensive review. Nutr Rev 54, 295-317 (1996).
- Falkingham, M., Abdelhamid, A., Curtis, P., et al. The effects of oral iron supplementation on cognition in older children and adults: a systematic review and meta-analysis. Nutr J 9, 4 (2010).
- World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System,. (World Health Organization, Geneva, 2011).
- O'Brien, S. Surveillance report 2021. (Canadian Blood Services, Ottawa, ON, 2021).
- Canadian Blood Services. Donor wellness and iron: ferritin testing. Vol. 2023 (https://www.blood.ca/en/blood/donating-blood/donor-health-and-safety/donor-wellness-and-iron-ferritin-testing, 2023).
- Cable, R.G., Glynn, S.A., Kiss, J.E., et al. Iron deficiency in blood donors: the REDS-II Donor Iron Status Evaluation (RISE) study. Transfusion 52, 702-711 (2012).
- Goldman, M., Uzicanin, S., Scalia, V., et al. Iron deficiency in Canadian blood donors. Transfusion 54, 775-779 (2014).
- Newman, B. Iron depletion by whole-blood donation harms menstruating females: the current whole-blood-collection paradigm needs to be changed. Transfusion 46, 1667-1681 (2006).
- Goldman, M., Uzicanin, S., Osmond, L., et al. A large national study of ferritin testing in Canadian blood donors. Transfusion 57, 564-570 (2017).
- Goldman, M., Uzicanin, S., Scalia, J., et al. Impact of informing donors of low ferritin results. Transfusion 56, 2193-2198 (2016).
- Baart, A.M., van Noord, P.A., Vergouwe, Y., et al. High prevalence of subclinical iron deficiency in whole blood donors not deferred for low hemoglobin. Transfusion 53, 1670-1677 (2013).
- Rigas, A.S., Sorensen, C.J., Pedersen, O.B., et al. Predictors of iron levels in 14,737 Danish blood donors: results from the Danish Blood Donor Study. Transfusion 54, 789-796 (2014).
- Salvin, H.E., Pasricha, S.R., Marks, D.C., et al. Iron deficiency in blood donors: a national cross-sectional study. Transfusion 54, 2434-2444 (2014).
- Mast, A.E., Bialkowski, W., Bryant, B.J., et al. A randomized, blinded, placebo-controlled trial of education and iron supplementation for mitigation of iron deficiency in regular blood donors. Transfusion 56, 1588-1597 (2016).
- Snook, J., Bhala, N., Beales, I.L.P., et al. British Society of Gastroenterology guidelines for the management of iron deficiency anaemia in adults. Gut 70, 2030-2051 (2021).
- Spencer, B.R., Bialkowski, W., Creel, D.V., et al. Elevated risk for iron depletion in high-school age blood donors. Transfusion 59, 1706-1716 (2019).
- Cable, R.G., Glynn, S.A., Kiss, J.E., et al. Iron deficiency in blood donors: the REDS-II Donor Iron Status Evaluation (RISE) study. Transfusion 52, 702-711 (2012).
- Patel, E.U., White, J.L., Bloch, E.M., et al. Association of blood donation with iron deficiency among adolescent and adult females in the United States: a nationally representative study. Transfusion 59, 1723-1733 (2019).
- Rigas, A.S., Sørensen, C.J., Pedersen, O.B., et al. Predictors of iron levels in 14,737 Danish blood donors: results from the Danish Blood Donor Study. Transfusion 54, 789-796 (2014).
- Bryant, B.J., Yau, Y.Y., Arceo, S.M., et al. Ascertainment of iron deficiency and depletion in blood donors through screening questions for pica and restless legs syndrome. Transfusion 53, 1637-1644 (2013).
- Cable, R.G., Brambilla, D., Glynn, S.A., et al. Effect of iron supplementation on iron stores and total body iron after whole blood donation. Transfusion 56, 2005-2012 (2016).