Emerging Artificial Intelligence Methods to Assess Transfusion Quality

Our partnership with the Centre for Blood Research (CBR) at the University of British Columbia is helping to train the next generation of researchers in transfusion science. This blog post highlights just some of the achievements accomplished by CBR trainees in education, training or knowledge mobilization.
Erik Lamoureux, a PhD Student from the Ma Lab (Multi-Scale Design Laboratory) at CBR and recipient of a Canadian Blood Services Graduate Fellowship award, provides a summary of his lab’s paper “Assessing red blood cell deformability from microscopy images using deep learning”. Below is an abridged version of the post that originally appeared on the Centre for Blood Research blog in November 2022.
Around half of all Canadians will require a blood transfusion in their lifetime or know someone else who will. Despite how common blood transfusions are, only four percent of Canadians are blood donors. Due to the scarcity of blood for transfusion, it is vital to use the existing blood supply as efficiently as possible. It is well known that blood type is assessed – O, A, B, or AB, with +/- Rhesus (Rh) factor – to ensure blood compatibility between the donor and recipient. In addition to blood type, recent research indicates that the shape and deformability of red blood cells (RBCs) are important factors contributing to the effectiveness of a blood transfusion.
Red blood cells and deformability
The deformability of red blood cells – their ability to squeeze through small spaces – is vital for their navigation through the body. During circulation, RBCs squeeze through small gaps in the microvasculature to deliver oxygen and remove carbon dioxide from cells and tissues. Not only do RBCs need to squeeze through these small gaps, but they must also do this repeatedly; they circulate through the body once every 60 seconds and endure for a 120-day life span. Due to this, RBC deformability is vital for effective circulation.
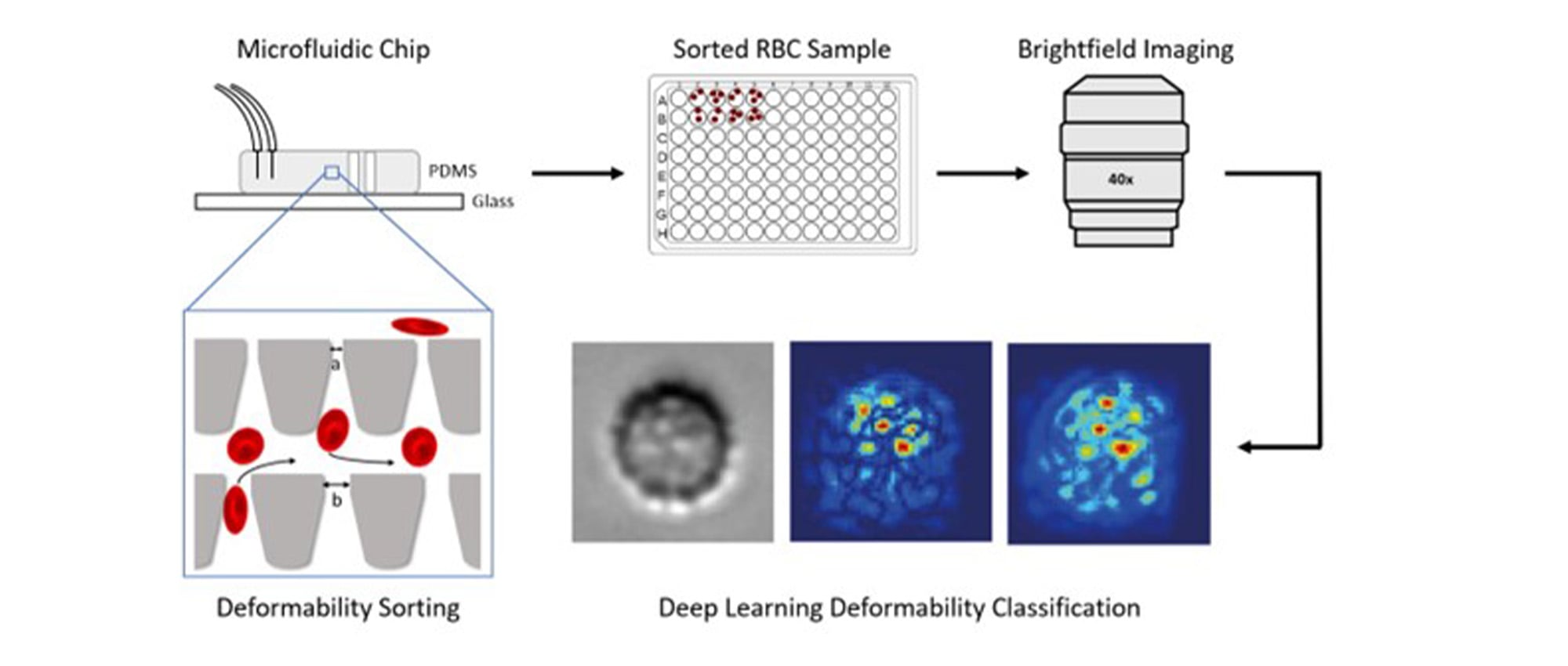
Figure 1. Red blood cells are sorted based on their deformability using a microfluidic device. The sorted cells are extracted, imaged, processed, and assessed using artificial intelligence (AI) image analysis methods called deep learning.
Why deformability matters
Red blood cell deformability degrades as the cell ages, and when the cell becomes too rigid to pass through the microvasculature, it is engulfed and destroyed by immune cells called phagocytes. Because of this relationship between a cell’s deformability and longevity, RBC deformability is considered a potential biomarker for transfusion quality. Ideally, blood banks could sort blood units based on patient need. More deformable and longer-lasting blood should be distributed to chronic transfusion patients to extend the time between their needed transfusions. On the other hand, more rigid and shorter-lasting blood should be distributed to acute transfusion patients (e.g., trauma patients) who just need a blood top-up and can otherwise produce an adequate blood supply.
In our lab, we developed a microfluidic device to sort RBCs based on their deformability1. RBCs suspended in fluid are sent through microchannels that are as small as the width of a human hair. The cells enter a grid-like sorting region consisting of small constrictions of different sizes for the cells to squeeze through. This sorting is similar to cells squeezing through small gaps in the body’s microvasculature. Based on a cell’s ability to squeeze through these gaps, they are sorted to different outlets indicating their level of deformability. This allows us to determine a donor-specific rigidity score and provides us with the true deformability levels of the cells for use in training a machine learning model.
Artificial intelligence (AI) to assess deformability
To increase the accessibility of determining RBC deformability, we sought to develop computer-based techniques to predict deformability from images. After microfluidic deformability sorting, sorted cells are extracted from the device and imaged using a microscope. The microscope captures digital images of the cells which are then processed into smaller single-cell images. These single cell images are input to an artificial intelligence model called a deep learning network. This network consists of cascading and interconnected mathematical operations that learn patterns in the data. By passing enough images through the network many times, the model is trained to identify a cell’s deformability level based on its surface features, patterns, and structures.
Benefits of artificial intelligence methods
Future work will focus on streamlining this procedure, determining viable use cases and limitations, and ideally developing a generalizable model that can assess the RBC deformability profile of new donors at the point of care.

Erik Lamoureux is a PhD Student from the Ma Lab (Multi-Scale Design Laboratory) at the Centre for Blood Research (CBR) at the University of British Columbia and a recipient of a Canadian Blood Services graduate fellowship award.
References
[1] Guo, Q. et al. Deformability based sorting of red blood cells improves diagnostic sensitivity for malaria caused by Plasmodium falciparum. Lab Chip 20, 645–654 (2016).